Gregory I Bain1, Ian J Galley2, Angus R.E Keogh1, Adam W Durrant1
1 Modbury Public Hospital, Modbury, South Australia,
2 Royal Adelaide Hospital, Adelaide, South Australia,
Correspondence Address:
Gregory I Bain
196 Melbourne St, North Adelaide, 5006, Australia
Login to access the Email id
Source of Support: None, Conflict of Interest: None
Abstract
Neurovascular complications have been reported from both plate osteosynthesis and intramedullary fixation of midshaft clavicle fractures. We wish to report a case of limb threatening ischemia from screw penetration of the axillary artery after plate osteosynthesis for a clavicle nonunion. A literature review of vascular trauma from midshaft clavicle fractures is presented.
Keywords: Clavicle, fracture, nonunion, pseudoaneurysm
How to cite this article:
Bain GI, Galley IJ, Keogh AR, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg 2010;4:79-82
How to cite this URL:
Bain GI, Galley IJ, Keogh AR, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg [serial online] 2010 [cited 2016 May 13];4:79-82. Available from: http://www.internationalshoulderjournal.org/text.asp?2010/4/3/79/76969
Introduction Top
Clavicle fractures are common, accounting for 5-12% of all fractures. [1],[2] The results of non-operative management of middle third clavicle fractures are typically good with a rate of nonunion between 0.1 and 5%. [1],[3],[4] Internal fixation of clavicle fractures in patients with a high risk of nonunion has been advocated. [5],[6],[7],[8],[9] Appreciation of the negative effect on shoulder function of clavicle shortening, [10],[11],[12] the availability of anatomy specific locking plates and intramedullary devices has also increased the popularity of clavicle fixation.
Neurovascular complications have been reported from both plate osteosynthesis [13],[14],[15] and intramedullary fixation of midshaft clavicle fractures. [16]
We wish to report a case of limb threatening ischemia from screw penetration of the axillary artery after plate osteosynthesis for a clavicle nonunion. A literature review of vascular trauma from midshaft clavicle fractures is presented.
Case Report Top
A 32-year-old male carpet layer suffered a closed fracture to his nondominant left clavicle in 1998. He was treated non-operatively and went on to develop a symptomatic nonunion. Open reduction and bone grafting of the nonunion was performed in 1999 with a six-hole AO small fragment dynamic compression plate (DCP) (Synthes® ).
The clavicle united and his symptoms resolved. He presented 6 years after his surgery, with 18 months of progressively worsening pain, paraesthesia and claudication in his left hand. In the week prior to presentation, he noticed that his left hand was cool and pale.
Clinically, he had a well-healed scar over his left clavicle with no associated mass or bruit. His left axillary artery was palpable. However, his brachial, radial and ulnar arteries were not. He had pain in the hand with exertion and poor capillary return. There were no trophic changes. His upper limb neurology was normal.
Plain radiographs demonstrated a united clavicle with a six-hole plate superiorly. The medial screw was prominent inferiorly [Figure 1].
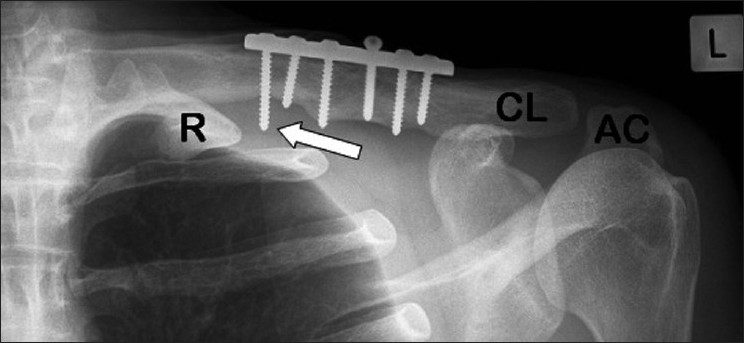 |
Figure 1: Plain radiograph of left clavicle. (AC: Acromion. CL: Clavicle. R: 1st rib). Arrow depicts prominent medial screw lateral to the 1st rib
Click here to view |
An arteriogram demonstrated the medial screw penetrating the axillary artery with an associated pseudoaneurysm [Figure 2]. There was occlusion of the brachial artery above the elbow [Figure 3] with slow filling of the ulnar artery via collateral vessels. The radial artery and the proximal one-third of the ulnar artery were occluded. There was little flow past the metacarpophalangeal (MCP) joints. A computed tomography (CT) arteriogram confirmed penetration of the axillary artery by the prominent medial screw, with an associated pseudoaneurysm [Figure 4] and [Figure 5].
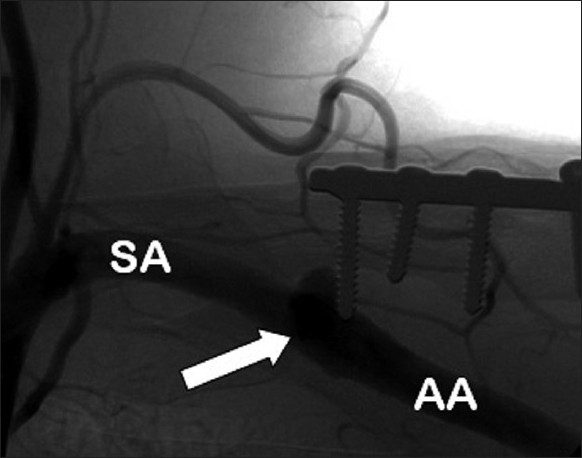 |
Figure 2: Arteriogram. AA: axillary artery. (SA: Subclavian artery). Arrow depicts penetration of the axillary artery by the prominent medial screw. A pseudoaneurysm has formed. The axillary artery is filled with contrast distal to the pseudoaneurysm
Click here to view |
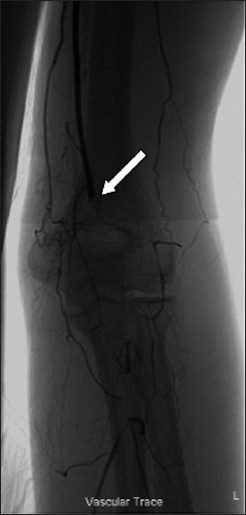 |
Figure 3: Arteriogram at level of left elbow. The arrow indicates occlusion of the brachial artery. Sluggish distal perfusion is provided via collateral vessels at the level of the elbow
Click here to view |
 |
Figure 4: CT arteriogram of left clavicle, demonstrating penetration of the axillary artery by the prominent medial screw with associated pseudoaneurysm of the axillary artery. All structures apart from the clavicle and subclavian and axillary arteries have been subtracted
Click here to view |
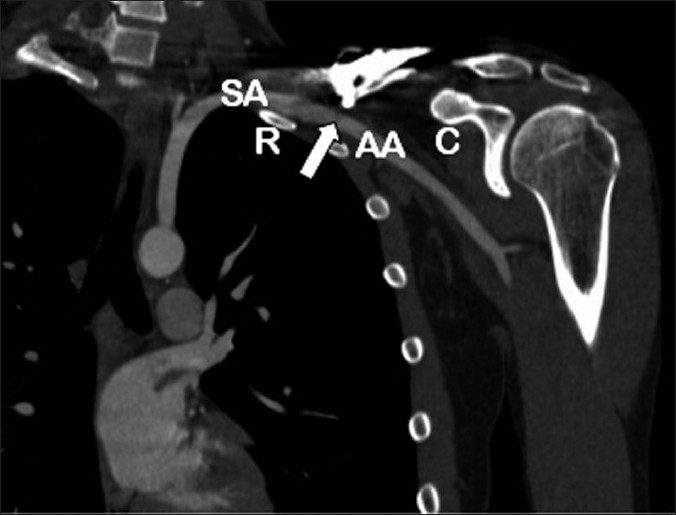 |
Figure 5: Coronal 2D reconstruction CT arteriogram of left shoulder. (AA: axillary artery; C: Coracoid process; R: 1st rib; SA: Subclavian artery). Arrow depicts prominent screw with associated pseudoaneurysm. The subclavian artery becomes the axillary artery at the lateral border of the first rib. The subclavian artery lies in a groove on the superior aspect of the 1st rib
Click here to view |
The patient was anticoagulated following plate removal [Figure 6]. The prominent medial screw measured 26 mm.
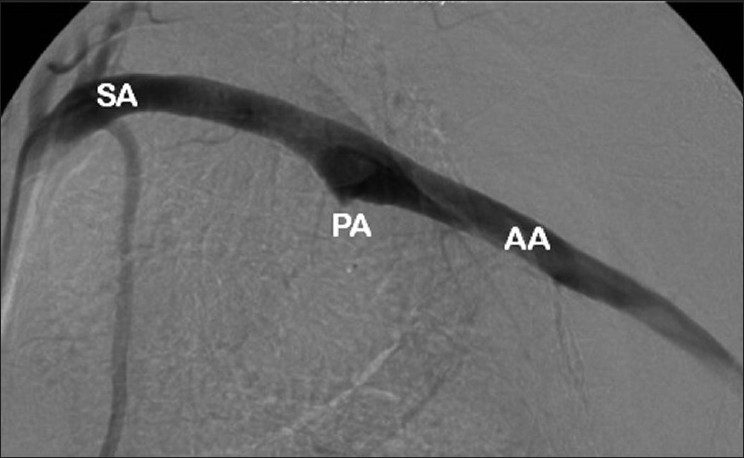 |
Figure 6: Arteriogram of left subclavian and axillary artery following removal of internal fixation. (AA: Axillary artery; PA: Pseudoaneurysm; SA: Subclavian artery)
Click here to view |
The pseudoaneurysm was bypassed using an 8 mm by 25 mm Viabahn® (W. L. Gore and Associates, Flagstaff, AZ, USA) stent placed in the axillary artery via a femoral approach. The self-expanding stent is constructed with a durable, reinforced biocompatible, expanded polytetrafluoroethylene (ePTFE) liner attached to the external nitinol stent structure.
The stent was dilated using a 7 mmΧ40 mm balloon [Figure 7].
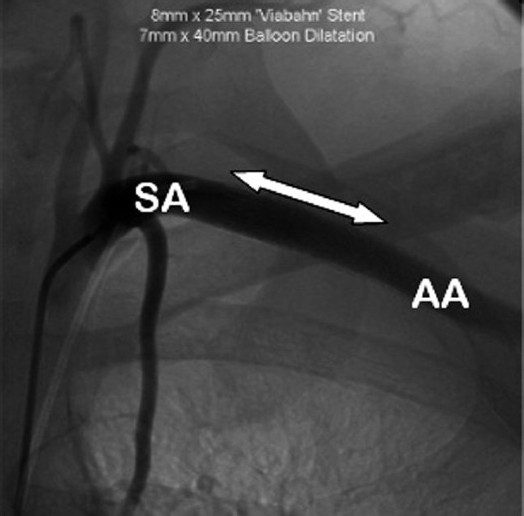 |
Figure 7: Arteriogram of left subclavian and axillary artery following insertion of 8 mm×25 mm Viabahn® (WL Gore, Flagstaff, AZ, USA) endoprosthesis, shown by arrow, after balloon dilation with 7 mm×40 mm balloon. ( AA: Axillary artery; SA: Subclavian artery). The neck of the pseudoaneurysm has been occluded
Click here to view |
Discussion Top
Iatrogenic vascular injury from internal fixation of midshaft clavicle fractures is rare, with only three other reported cases from plate osteosynthesis. Johnson [14] reported a case of left arm ischemia presenting 22 months after internal fixation of an acute fracture. A pseudoaneurysm with occlusion of the brachial artery was found. Ligation of the subclavian artery followed by carotid-axillary bypass grafting resulted in a symptom-free left arm.
Casselman [13] reported a similar case, 8 years following internal fixation of a nonunion. The pseudoaneurysm and first rib was resected via a transclavicular approach. Interposition grafting was performed using Gor-Tex (W. L. Gore and Associates, Flagstaff, AZ, USA). The clavicle was bone grafted and internally fixed at the end of the procedure.
Shackford [15] reported a case, 10 years following internal fixation of a midshaft nonunion. Angiography confirmed a pseudoaneurysm with screw penetration of the subclavian artery and occlusion of the brachial artery. Resection of the pseudoaneurysm confirmed screw penetration of the artery. Interposition vein grafting and claviculectomy gave a good clinical result.
All cases had a delayed presentation ranging from 22 months to 10 years following internal fixation. It is possible that the prominent screw erodes through the arterial wall with shoulder movement. Another explanation is that the artery is injured at the time of injury or surgery and forms a pseudoaneurysm, which was found in all cases. The upper limb has an extensive collateral circulation [17] particularly around the shoulder and elbow. This allowed all four patients to present with claudication symptoms rather than critical ischemia despite occlusion of the brachial artery.
There have been multiple reported cases of vascular injuries from midshaft clavicle fractures. [18],[19],[20],[21],[22],[23],[24] These include arterial and venous lacerations and arterial pseudoaneurysms. [25],[26],[27],[28],[29],[30],[31],[32] Death from vascular injury secondary to clavicle fracture has been reported. [33],[34] The most famous case is that of Sir Robert
Peel (1788-1850) who created the police force in Great Britain. Subclavian vein thrombosis (Paget-Schroetter’s syndrome) [35],[36],[37] from clavicle fracture and pulmonary emboli from this thrombus [38] has been reported.
Nonoperative treatments for psuedoaneurysms, such as external ultrasound compression and transcatheter coiling,
have been used at other sites. However, they are not suitable for the subclavian artery. Ultrasound guided thrombin injections have been successfully used for a subclavian pseudoaneurysm. [39] There is, however, a risk of occluding one of the branches supplying cerebral circulation.
Surgical treatment can be performed by means of a supraclavicular incision and can be combined with clavicular resection. Access to the proximal subclavian artery may require a median sternotomy or a thoracotomy through the third or fourth intercostal space on the left. [18],[20]
Endovascular stenting, as was used in this case, has been used previously for pseudoaneurysm associated with a clavicle fracture. [29],[40] It has the advantage of being minimally invasive with a remote access site. Potential problems include late stenosis and fracture of the stents. Newer flexible drug eluting stents may prevent this problem. [29]
This case reminds us of the importance of careful screw placement for osteosynthesis of the clavicle. The proximity of the clavicle and subclavian artery has previously been described [41] and it is suggested that screws for osteosynthesis of the clavicle be no longer than 18 mm in order to avoid the subclavian artery. Pseudoaneurysm of the subclavian artery in this instance was successfully treated with a closed procedure. However, there is the potential for significant morbidity.
Acknowledgments
The authors would like to acknowledge Ron Heptinstall RN and the Modbury Hospital Foundation for help in preparation of this manuscript.
References
Basamania C, Craig E, Rockwood CJ. Fractures of the clavicle. In: Rockwood C, Matsen III F, Wirth M, editors. The Shoulder. Philadelphia: WB Saunders Co; 2004. p. 455. Back to cited text no. 1
2. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res 1968;58:29-42. Back to cited text no. 2
[PUBMED]
3. Neer CS 2 nd . Nonunion of the clavicle. J Am Med Assoc 1960;172:1006-11. Back to cited text no. 3
4. Robinson CM. Fractures of the clavicle in the adult: Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. Back to cited text no. 4
[PUBMED] [FULLTEXT]
5. Brinker MR, Edwards TB, O’Connor DP. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2005;87:676-7. Back to cited text no. 5
6. Gossard JM. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1998;80:558. Back to cited text no. 6
[PUBMED] [FULLTEXT]
7. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. Back to cited text no. 7
[PUBMED] [FULLTEXT]
8. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86-A:1359-65. Back to cited text no. 8
[PUBMED] [FULLTEXT]
9. Wick M, Muller EJ, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg 2001;121:207-11. Back to cited text no. 9
10. Chan KY, Jupiter JB, Leffert RD, Marti R. Clavicle malunion. J Shoulder Elbow Surg 1999;8:287-90. Back to cited text no. 10
[PUBMED]
11. Ledger M, Leeks N, Ackland T, Wang A. Short malunions of the clavicle: An anatomic and functional study. J Shoulder Elbow Surg 2005;14:349-54. Back to cited text no. 11
[PUBMED] [FULLTEXT]
12. McKee MD, Wild LM, Schemitsch EH. Midshaft malunions of the clavicle. J Bone Joint Surg Am 2003;85-A:790-7. Back to cited text no. 12
[PUBMED] [FULLTEXT]
13. Casselman F, Vanslembroek K, Verougstraete L. An unusual cause of thoracic outlet syndrome. J Trauma 1997;43:142-3. Back to cited text no. 13
[PUBMED] [FULLTEXT]
14. Johnson B, Thursby P. Subclavian artery injury caused by a screw in a clavicular compression plate. Cardiovasc Surg 1996;4:414-5. Back to cited text no. 14
[PUBMED] [FULLTEXT]
15. Shackford SR, Connolly JF. Taming of the screw: A case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma 2003;55:840-3. Back to cited text no. 15
[PUBMED] [FULLTEXT]
16. Ring D, Holovacs T. Brachial plexus palsy after intramedullary fixation of a clavicular fracture. A report of three cases. J Bone Joint Surg Am 2005;87:1834-7. Back to cited text no. 16
[PUBMED] [FULLTEXT]
17. Levin PM, Rich NM, Hutton JE Jr. Collaternal circulation in arterial injuries. Arch Surg 1971;102:392-9. Back to cited text no. 17
[PUBMED] [FULLTEXT]
18. Costa MC, Robbs JV. Nonpenetrating subclavian artery trauma. J Vasc Surg 1988;8:71-5. Back to cited text no. 18
[PUBMED]
19. Howard FM, Shafer SJ. Injuries to the clavicle with neurovascular complications. A study of fourteen cases. J Bone Joint Surg Am 1965;47:1335-46. Back to cited text no. 19
[PUBMED]
20. Katras T, Baltazar U, Rush DS, Davis D, Bell TD, Browder IW, et al. Subclavian arterial injury associated with blunt trauma. Vasc Surg 2001;35:43-50. Back to cited text no. 20
[PUBMED]
21. Klier I, Mayor P. Laceration of the innominate internal jugular venous junction: Rare complications of fracture of the clavicle. Orthop Rev 1981;10:81-2. Back to cited text no. 21
22. Natali J, Maraval M, Kieffer E, Petrovic P. Fractures of the clavicle and injuries of the sub-clavian artery. Report of 10 cases. J Cardiovasc Surg (Torino) 1975;16:541-7. Back to cited text no. 22
[PUBMED]
23. Penn I. The vascular complications of fractures of the clavicle. J Trauma 1964;4:819-31. Back to cited text no. 23
[PUBMED]
24. Tse DH, Slabaugh PB, Carlson PA. Injury to the axillary artery by a closed fracture of the clavicle. A case report. J Bone Joint Surg Am 1980;62:1372-4. Back to cited text no. 24
[PUBMED]
25. Cayford EH, Tees FJ. Traumatic aneurysm of the subclavian artery as a late complication of fractured clavicle. Can Med Assoc J 1931;25:450-2. Back to cited text no. 25
[PUBMED] [FULLTEXT]
26. Debakey ME, Beall AC Jr, Wukasch DC. Recent developments in vascular surgery with particular reference to orthopaedics. Am J Surg 1965;109:134-42. Back to cited text no. 26
[PUBMED]
27. Gryska PF. Major vascular injuries. Principal of management in selected cases of arterial and venous injury. N Engl J Med 1962;266:381-5. Back to cited text no. 27
[PUBMED] [FULLTEXT]
28. Hansky B, Murray E, Minami K, Korfer R. Delayed brachial plexus paralysis due to subclavian pseudoaneurysm after clavicular fracture. Eur J Cardiothorac Surg 1993;7:497-8. Back to cited text no. 28
29. Renger RJ, de Bruijn AJ, Aarts HC, van der Hem LG. Endovascular treatment of a pseudoaneurysm of the subclavian artery. J Trauma 2003;55:969-71. Back to cited text no. 29
[PUBMED] [FULLTEXT]
30. Serrano JA, Rodriguez P, Castro L, Serrano P, Carpintero P. Acute subclavian artery pseudoaneurysm after closed fracture of the clavicle. Acta Orthop Belg 2003;69:555-7 Back to cited text no. 30
31. Shih JS, Chao EK, Chang CH. Subclavian pseudoaneurysm after clavicle fracture. Taiwan Yi Xue Hui Za Zhi 1983;82:332-5. Back to cited text no. 31
[PUBMED]
32. Yates DW. Complications of fractures of the clavicle. Injury 1976;7:189-93. Back to cited text no. 32
[PUBMED] [FULLTEXT]
33. Dickson J. Death following fractured clavicle. BMJ 1952;2:666 Back to cited text no. 33
34. Kendall KM, Burton JH, Cushing B. Fatal subclavian artery transection from isolated clavicle fracture. J Trauma 2000;48:316-8. Back to cited text no. 34
[PUBMED] [FULLTEXT]
35. Hughes ES. Venous obstruction in the upper extremity; Paget-Schroetter’s syndrome; a review of 320 cases. Surg Gynecol Obstet 1949;88:89-127. Back to cited text no. 35
[PUBMED]
36. Lim EV, Day LJ. Subclavian vein thrombosis following fracture of the clavicle. A case report. Orthopedics 1987;10:349-51. Back to cited text no. 36
[PUBMED]
37. Steinberg I. Subclavian vein thrombosis associated with fractures of the clavicle. N Engl J Med 1961;264:686-8. Back to cited text no. 37
38. Scarpa FJ, Levy RM. Pulmonary embolism complicating clavicle fracture. Conn Med 1979;43:771-3. Back to cited text no. 38
[PUBMED]
39. McConnell PI, Rehm J, Oltman DL, Lynch TG, Baxter BT. Thrombin injection for treating a subclavian artery pseudoaneurysm. Surgery 2000;127:716-8. Back to cited text no. 39
[PUBMED] [FULLTEXT]
40. Pfammatter T, Kunzli A, Hilfiker PR, Schubiger C, Turina M. Relief of subclavian venous and brachial plexus compression syndrome caused by traumatic subclavian artery aneurysm by means of transluminal stent-grafting. J Trauma 1998;45:972-4. Back to cited text no. 40
41. Galley IJ, Watts AC, Bain GI. The anatomic relationship of the axillary artery and vein to the clavicle: A cadaveric study. J Shoulder Elbow Surg 2009;18:e21-5. Back to cited text no. 41
Figures
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
This article has been cited by
1 Endobypass using a heparin-bonded covered stent to treat upper limb claudication due to axillary artery occlusion following axillofemoral bypass
Chaudhuri, A.
EJVES Extra. 2012; 23(5): e48-e49
[Pubmed]
2 Endobypass Using a Heparin-bonded Covered Stent to Treat Upper Limb Claudication due to Axillary Artery Occlusion Following Axillofemoral Bypass
A. Chaudhuri
EJVES Extra. 2012; 23(5): e48
[Pubmed] | [DOI]
