Abstract
Limb salvage is now the norm for a large majority of malignant bone tumors. The proximal humerus is the third most common site for the occurrence of malignant tumors of bone. In tumors of the proximal humerus with large volume disease, extensive involvement of the diaphysis is not infrequent. Resection may often extend as far as the distal metaphysis in order to obtain adequate oncologic margins. A very small distal stump of bone poses unique challenges in reconstruction where conventional reconstruction modalities may be difficult to apply. We describe the use of a customised plate to reconstruct these defects which offers an inexpensive, easy to use, durable reconstruction option. It provides adequate shoulder and arm stability and ensures excellent hand and elbow motion with good functional results.
Introduction
Limb salvage is now the norm for a large majority of malignant bone tumors. Advances in imaging and the development of effective adjuvant modalities have made limb salvage an oncologically safe option without compromising on long-term survival. Various techniques have been advocated for reconstruction of skeletal defects after limb salvage.
The proximal humerus is the third most common site for the occurrence of malignant tumors of the bone. In tumors of the proximal humerus with large volume disease, extensive involvement of the diaphysis is not infrequent. Resection may often extend as far as the distal metaphysis in order to obtain adequate oncological margins. A very small distal stump of bone poses unique challenges in reconstruction.
Reconstruction with conventional prosthesis is not possible because of the short residual stump. [1] We describe the use of an inexpensive custom made plate to reconstruct these defects. It provides adequate shoulder and arm stability and ensures excellent hand and elbow function.
Technique
The primary goal of surgery is complete excision of the tumor, with preservation of the limb. A 2 to 3 cm marrow margin, as calculated on the T1 weighted MRI image, is considered an adequate resection margin. In tumors of the proximal humerus with extensive involvement of the diaphysis, where the resection extends as far as the distal metaphysis, a very small residual distal stump of bone remains. The distal stump of the bone is usually adequate to allow two (occasionally three) cortical screws to pass through a plate into the bone.
Based on preoperative planning, a customized plate (Sushrut Surgicals, Devrukh, India) is ordered. The length of the plate depends on the length of the bone resected plus an additional two or three screw holes (depending on the length of the residual distal stump of the bone). Unlike conventional internal fixation plates this plate is solid except for one screw hole proximally and two / three screw holes distally [Figure 1]. It is also 33% thicker than the conventionally used plates and made of vacuum-remelted stainless steel.
![]() Figure 1: Customized plate. Arrow highlights the proximal hole through which the polypropylene mesh is passed
Figure 1: Customized plate. Arrow highlights the proximal hole through which the polypropylene mesh is passed
After the tumor is resected the plate is anchored to the distal bone stump with bicortical screws passed through the distal holes [Figure 2]. Polymethylmethacrylate bone cement is digitally packed into the medullary canal of the short distal stump to improve the quality of the screw hold. A commercially available polypropylene mesh (Prolene TM – Johnson and Johnson) is passed through the proximal hole and anchored circumferentially to the glenoid with the help of four to six sutures passed through bone, using No: 2 Ethibond Excel TM (Johnson and Johnson), a polyester braided nonabsorbable material. The mesh also serves as an anchor for any residual capsule or para-articular soft tissue. [2]
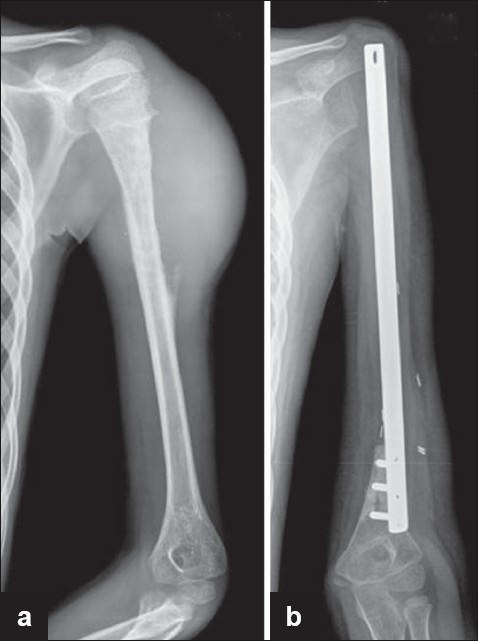
Figure 2: (a) Radiograph showing Ewing’s sarcoma of the proximal humerus (b) Radiograph showing reconstruction with the customised plate
Results
Since January 2006 we have used this technique in eight patients [Table 1]. The follow up for survivors ranges from 10 months to 33 months (mean 20.5 months). Except for the first case, in whom a conventional reconstruction plate was used which broke at 13 months [Figure 3] we have not had any implant complications.
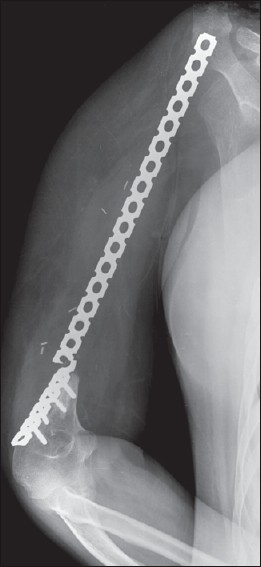
Figure 3: Plate breakage (case: 1) at 13 months when a conventional reconstruction plate was used
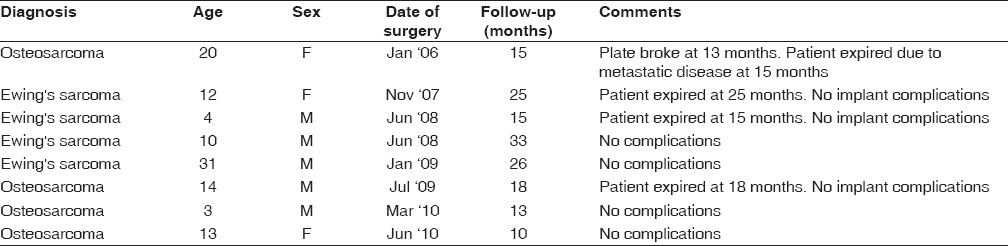 Table 1: Patient details
Table 1: Patient details
Discussion
Achieving adequate oncological margins is the cornerstone of successful limb salvage surgery. It would be imprudent to compromise on tumor resection in order to facilitate subsequent reconstruction. Reconstructing large resection gaps following tumor resection has always been challenging. The problem is further compounded if the distal stump of bone is very small. Endoprostheses, the most common mode of reconstruction need a definite amount of residual host bone for adequate fixation of the stem after resection, and this is a limiting factor to their use in such cases. [1] Although resection of the entire bone and replacement with a total humeral prosthesis is an option, it is preferable to retain the native elbow joint for durable long-term elbow function.
Strut allografts although useful options are limited by their availability and are associated with nonunion, fracture, and infection, besides the fear of disease transmission. Vascularized autografts require specialized surgical skills and have their own complications and associated morbidity.
Most authors agree that after reconstruction of extensive proximal humeral lesions the shoulder function is compromised. [3],[4] Stability at the proximal end of the reconstruct ensures good hand and elbow function. Reconstructing these defects using this custom-made plate is an inexpensive (the plate costs US $60) and effective method, which gives adequate shoulder and arm stability and ensures excellent hand and elbow function [Figure 4]. The complications in bone graft incorporation due to the use of adjuvant chemotherapy and radiotherapy leading to a delay in postoperative rehabilitation are avoided with a metallic implant. Although the number of screws through the distal fragment is limited, the use of bone cement helps improve the quality of the screw hold. [5],[6] The solid, thicker plate made of vacuum-remelted stainless steel increases the strength of the implant, thus reducing the incidence of implant failure. Titanium locking plates utilized in orthopedic trauma can be used as an alternative, but they are considerably more expensive than the plate we have described. Unlike the lower limb, which is subject to variable stresses and loading, the upper limb faces relatively less intense biomechanical forces, and this could be the reason why none of the reconstructs with the custom-made, solid, thicker plates has needed revision so far. Failure of any implant in long-term oncology survivors is to be expected. If necessary, subsequent revision with a similar implant or biological methods is possible and should have good results, as these patients would at that stage be immunocompetent and free from the adverse effects of adjuvant therapy.
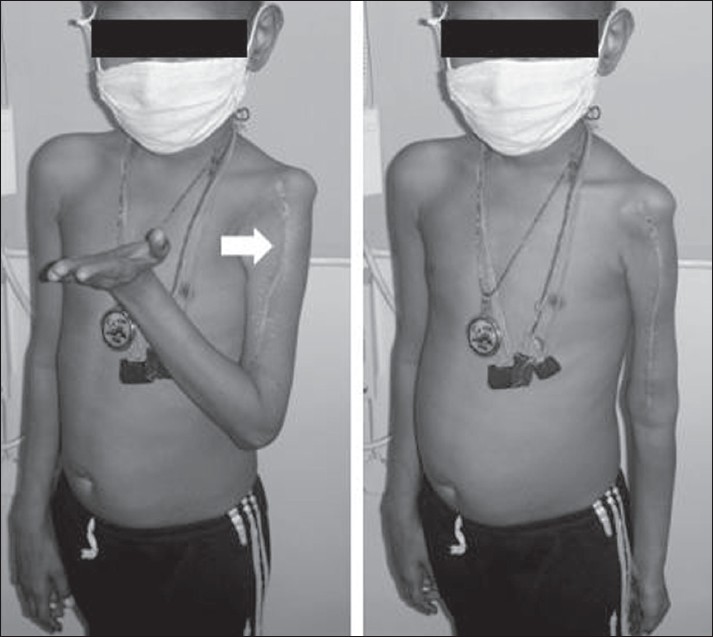
Figure 4: Postoperative elbow and hand function. Arrow highlights the long surgical scar
Conclusion
When evaluating a reconstruction technique we need to consider the ease of the procedure, its complications, functional outcome, and the durability of the reconstruct. Although a longer follow-up would be ideal, this technique provides an inexpensive, easy-to-use, durable reconstruction option, to reconstruct defects after resection in tumors of the proximal humerus, with extensive involvement of the diaphysis and with good functional results.
