1 Department of Orthopaedic Surgery, Concordia Hospital for Special Surgery, Rome, Italy
2 Department of Radiology, Universita’ di Roma La Sapienza, Rome, Italy
Correspondence Address
Abstract
Aims: One of the reason for Latarjet procedure failure may be coracoid graft osteolysis. In this study, we aimed to understand if a better compression between the coracoid process and the glenoid, using a mini-plate fixation during the Latarjet procedure, could reduce the amount of coracoid graft osteolysis.
Materials and Methods: A computed tomography scan analysis of 26 prospectively followed-up patients was conducted after modified Latarjet procedure using mini-plate fixation technique to determine both the location and the amount of coracoid graft osteolysis in them. We then compared our current results with results from that of our previous study without using mini-plate fixation to determine if there is any statistical significant difference in terms of corcacoid bone graft osteolysis between the two surgical techniques.
Results: The most relevant osteolysis was represented by the superficial part of the proximal coracoid, whereas the deep part of the proximal coracoid graft is least involved in osteolysis and has best bone healing. The current study showed a significant difference only for the deep part of the distal coracoid with our previous study (P < 0.01).
Discussion: To our knowledge, there are no studies in literature that show the causes of coracoid bone graft osteolysis after Latarjet procedure.
Conclusion: Our study suggests that there is a significant difference only for the deep part of the distal coracoid in terms of osteolysis. At clinical examination, this difference did not correspond with any clinical findings.
Level of Evidence: Level 4.
Clinical Relevance: Prospective case series, Treatment study.
Keywords: Bone graft, coracoid, istability, latarjet, osteolysis, shoulder
Introduction
Coracoid bone graft transfer is successful for antero-inferior shoulder stabilization with an extremely low failure rate. [1],[2],[3],[4],[5] We believe, as in literature, that the causes of Latarjet procedure failure (recurrent dislocation, subtle instability, pain, and stiffness) could be due to coracoid bone graft osteolysis and fibrous union. [1],[2],[3],[5],[6],[7],[8],[9],[10] We previously published a study on coracoid bone graft osteolysis after the Latarjet procedure, [11] wherein we showed that the part most involved in osteolysis is the superficial part of the proximal coracoid bone graft. In this study, we modified the Latarjet procedure by using a mini-plate fixation technique to improve the compression between the coracoid graft and the glenoid hoping to reduce the amount of coracoid bone graft osteolysis. The aim of this study was to determine if there is any statistical significant difference in terms of corcacoid bone graft osteolysis between our two surgical techniques for coracoid bone graft fixation (using mini-plate fixation or using screws and washer) [Figure 1].
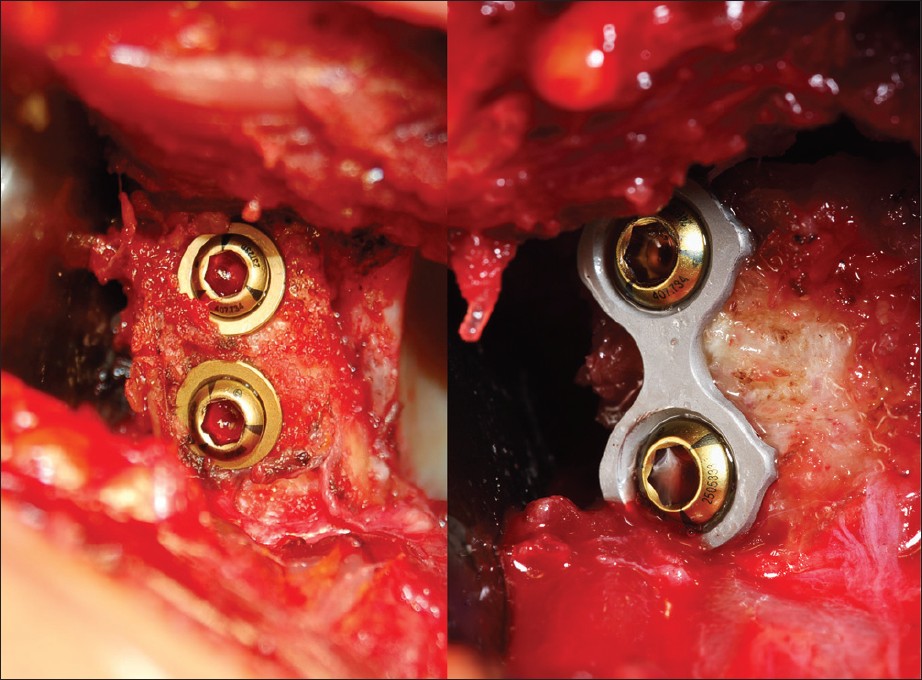
Figure 1: Final view of latarjet procedure using mini-plate fixation or using screws and washer
Materials and Methods
The inclusion criteria were recurrent antero-inferior dislocation with or without ligamentous hyperlaxity. The exclusion criteria were concomitant rotator cuff lesion, previous surgery for recurrent antero-inferior dislocation, and multidirectional instability. High-risk sports and activities were not exclusion criteria. The Latarjet procedure was performed for patients with a score of over 6 points (average 8 points) according to the Instability Severity Index Score (ISIS) (range of values 0-10), as described by Boileau. [12]
From May 2009 to February 2010, the authors prospectively followed-up 26 consecutive patients after the modified Latarjet procedure with the mini-plate fixation technique. Out of the 26 patients, 21 were men. The mean age of the patients was 31 ± 9 years. There were 13 right and left shoulders involved. In 12 patients, the surgery involved their dominant side (46.1%). Total 23 patients had more than one event of antero-inferior shoulder dislocation (average 6 ± 5.3 dislocations), 14 patients (53.8%) had 2-5 dislocations, 7 (26.9%) had 6-15 dislocations, and 2 (7.7%) had more than 15 dislocations. Total 16 (61.5%) patients were professional competitive sportsman involved in high demand sports like rugby, basket ball, boxing, and soccer. All patients had a positive apprehension and relocation test preoperatively. Total 11 patients (42.3%) gave positive Gagey test and 5 patients (19.2%) had positive Sulcus sign. All patients also had a standard range of motion: Mean active forward elevation was 178.1 ± 3.2 degrees, mean external rotation with the arm at the side was 47.4 ± 12.7 degrees. Also, 2 patients (7.7%) had an external rotation over 85 degrees and 5 patients (19.2%) had glenoid bone loss as quantified by the Pico method. [13] The average of glenoid bone loss was 16.6% (range 15-25%).
Preoperative plain X-ray studies were performed in the standard views including antero-posterior view, internal rotation view, external rotation view, lateral view, axillary view, and Bernageau view. Preoperative CT scans were performed for all patient prior to surgery for a better evaluation of the glenoid bone surface. [13]
Our surgical technique is a modified Latarjet procedure using a mini-plate [Figure 2] developed by the authors. This procedure is performed using a local bone graft by the osteotomy of the terminal 2 cm of the coracoid process, detaching the insertion of the pectoralis minor tendon. The coracoid bone graft is decorticated in the inferior surface until cancellous bone. After the split of the subscapularis tendon, the coracoid bone graft is transplanted along with the conjoined tendon to the antero-inferior glenoid rim that is decorticated. [14] The coracoid bone graft is positioned below the equator and no less than 2 mm from the glenoid cartilage. The coracoid bone graft is laid lengthwise and held in place with two bicortical cannulated screws partially threated (diameter 4 mm). In the modified Latarjet procedure, instead of using two washers, the authors used a mini-plate to improve the compression between the coracoid bone graft and the antero-inferior surface of the glenoid rim.
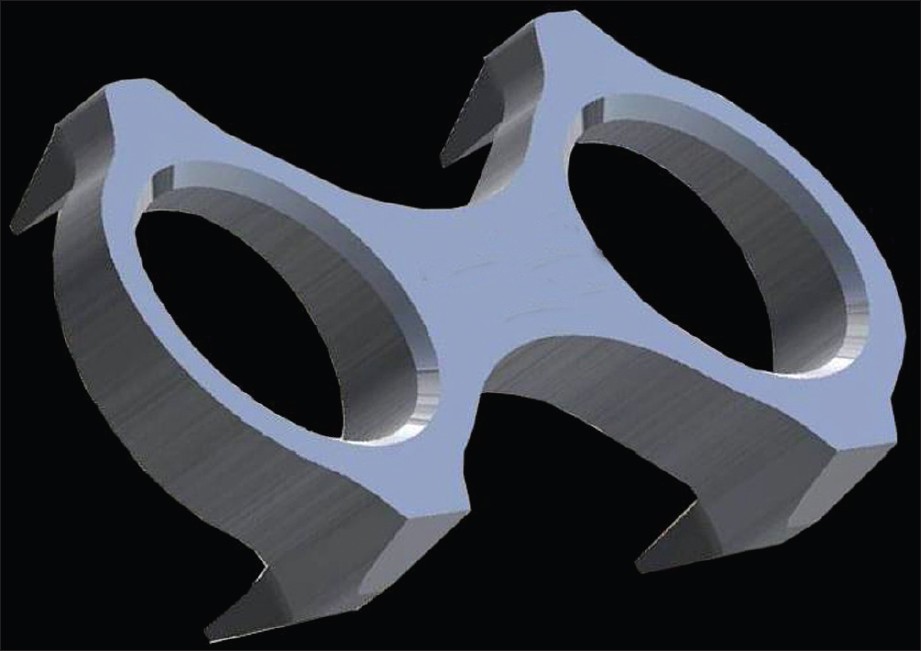
Figure 2: Modified latarjet procedure using a mini-plate
The mini-plate design has specific characteristics, each of which corresponds to a biomechanical function. It has a wedged profile. The wedge plate if placed medially on the slope on the medial scapular neck under compression, makes the coracoid bone graft rotate medially, thereby improving the bone match between the coracoid bone graft and the glenoid bone surface [Figure 3]. It has a figure of eight (8) configuration that allows a better torsional orientation of the plate on the dorsal-sloped coracoid surface. Four spikes for an improved stabilisation of the plate-bone block and two screw holes for lag screws insertion. These features allow the plate to distribute the load evenly to the bone.
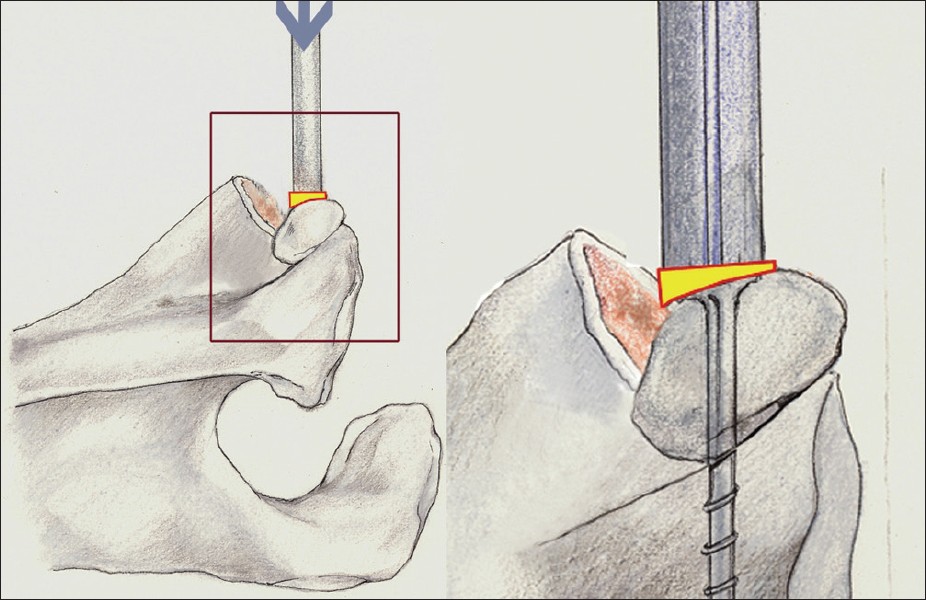
Figure 3: Bone match between the coracoid bone graft and the glenoid bone surface using mini-plate fixation
Postperative plain X-ray studies were performed in antero-posterior and lateral views to evaluate the correct position of the bone graft and the screws. A computed tomography (CT) scan evaluation with three-dimensional reconstruction was then performed in all patients to evaluate the coracoid bone graft 3 days after the surgery. A latest generation 64 slice CT scan (Siemens Somatom dual source scanner, 200 mA, 120 Kvp, slice thickness 1 mm) was used in this study. Similar to our previous study, the coracoid bone graft was divided into 8 parts. The two major regions were superficial and deep, which, in turn, was each divided into proximal, distal, medial, and lateral [Figure 4]. We measured the area of the mid portion over the superior screw (4 proximal parts) and under the inferior screw (4 distal parts) in the CT scan axial cut using a semi-automated edge detection module (Adobe Photoshop 7.0), according to the method described by Puri et al., [15] and Whang et al., [16] The areas of the 8 parts of the coracoids bone graft were calculated by determining the number of pixels/cm 2 . The CT scans were taken with a metal-artifact minimization. According to a previous study, the glenoid apex (the highest part of the glenoid) was used as a reference point during CT scan evaluation after surgery to ensure constant measurement during the follow-up CT scan assessment. [11]
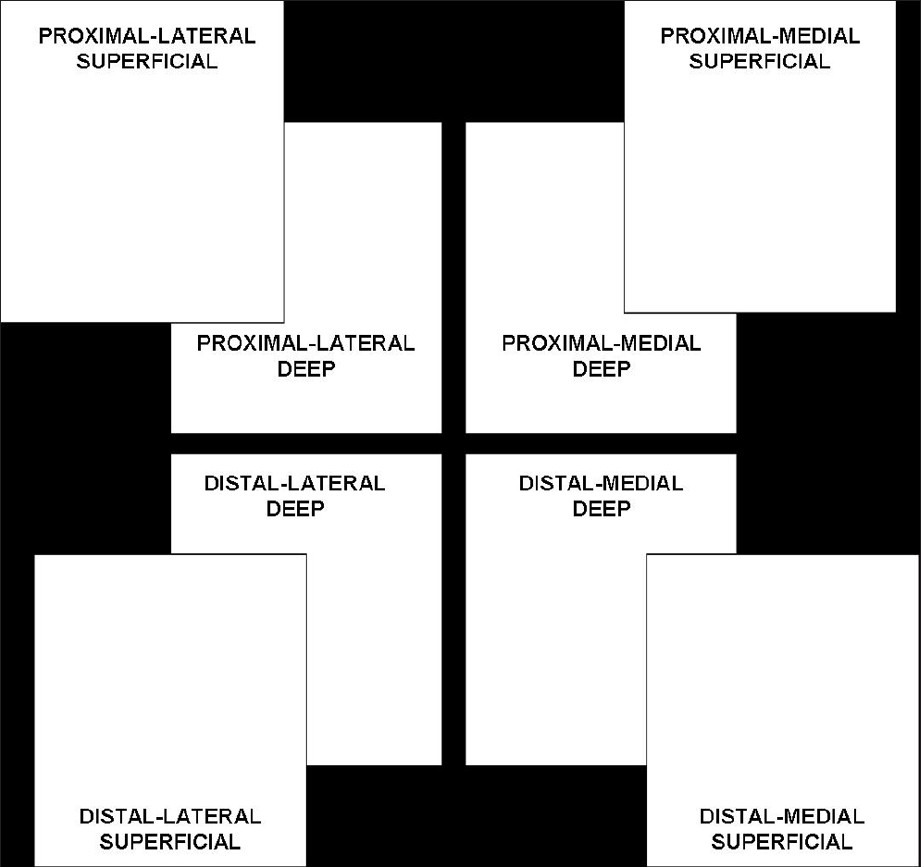
Figure 4: Diagram of partitioning in 8 parts of the coracoid bone graft in right shoulder (frontal view)
A second post-surgery CT scan assessment with three-dimensional reconstruction was then done at a mean period of 26 ± 3 months. No X-ray study was performed, because it is not as accurate as the CT scan for the evaluation of the coracoid graft osteolysis. The same method as described above was used for the follow-up study. The area of the 8 parts of the coracoid bone graft was measured as described and compared with the previous measurements done at 3 days post-surgery. All CT scans measurements were made by an independent radiologist who did not participate in the study.
During the follow-up, the authors also determined the functional status, range of motion, and the stability of the treated shoulder by means of two functional scoring systems: The Rowe score and the Walch Duplay score. A simple shoulder test (SST) was also performed on all patients.
Statistical analysis was performed by STATISTICA 7.0 software (StatSoft Inc., Tulsa, OK, USA). Database constituted of 26 patients defined by the percentage of osteolysis of the 8 coracoid parts. To normalize this rough data, we scaled the percentage values (v) into angular values (φ), from 0° to 90°, by the formula:
![]()
This trigonometric transformation allows magnification of the differences at the end of the scale (around 0% and 100% of osteolysis) because it is more relevant for a difference between 90% and 100% of osteolysis than between 50% and 60% of osteolysis. Moreover, this transformation has the advantage of returning variance ratios toward homoscedasticity values. Considering the 8 parts as related between them, we performed an analysis of variance (ANOVA) for repeated measures and then managed the post hoc confrontations (Bonferroni test, P < 0.01) between the osteolysis percentages of the 8 coracoid parts.
At the end, we matched (Student T test; P < 0.01) the normalized mean reabsorption value of the 8 parts individually with that of the homologue part of the previous study, without considering the relations between the 8 parts.
We then compared our current results with the results from that of our previous study without using mini-plate fixation to determine if there is any statistical significant difference in terms of corcacoid bone graft osteolysis between the two surgical techniques for coracoid bone graft fixation.
Results
The mean follow-up period for the 26 patients treated with the modified Latarjet procedure was 26 ± 3 months (the minimal follow-up was 18 months). Postoperative clinical examination revealed a mean active forward elevation of 174.7 ± 5.2 degrees (loss of average 3.4 degrees) and a mean external rotation with the arm at the side of 45.6 ± 10.3 degrees (loss of average 1.8 degrees), as measured by a standard goniometer.
According to the Rowe score, 16 (61.5%) patients had an excellent result (90-100 points), 9 (34.6%) had a good result (75-89 points), and only 1 (3.8%) had fair result (51-74 points). No patient had a poor result (<50 points).
According to the Walch Duplay score, 13 (50%) patients had an excellent result (91-100 points), 11 (42.3%) had a good result (76-90 points), 2 (7.7%) had a medium result (51-75 points), and no patient had a poor result (≤50 points).
The SST showed that most of the patients (96.1%) were satisfied after surgery, especially in daily activities as well as work or sports. No failure has been reported in this study (recurrent dislocation, subtle instability, pain, and stiffness).
Using CT scan analysis, we were able to study the evolving progress of coracoid bone graft osteolysis in the described 8 parts of the coracoid bone graft. The most relevant mean osteolysis percentage was represented by the superficial and medial part of the proximal coracoid bone graft (88.2 ± 21.4%) and by the superficial and lateral part of the proximal coracoid bone graft (80.6 ± 25.4%). The part with the least amount of osteolysis were the deep and lateral portion of the proximal coracoid bone graft (39.2 ± 39.7%) and the deep and medial portion of the proximal coracoid bone graft (54.2 ± 33.4%) [Table 1] and [Table 2]. On an average, 63.9% of the entire coracoid bone graft underwent osteolysis.

Table 1: Descriptive percentage of osteolysis for the 8 parts of the coracoids process in the 26 patients
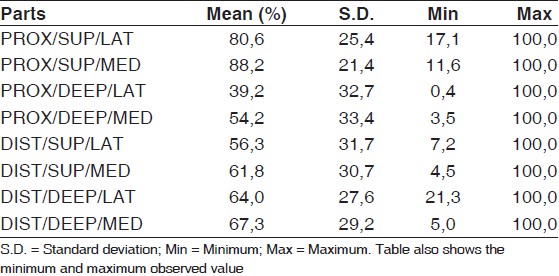 Table 2: Mean percentage and standard deviation of the reabsorption for the 8 parts of the coracoid.
Table 2: Mean percentage and standard deviation of the reabsorption for the 8 parts of the coracoid.
ANOVA for repeated measures showed a significant effect both for the between variance (F 1,25 = 361.3; P < 0.01) and for within variance (F 7,175 = 12.2; P < 0.01). The differences between the normalized mean osteolysis percentages of the 8 parts are reported in [Table 3]. In particular, we noticed that the proximal, superficial, and medial parts were significantly different in respect of every other part (row B; P < 0.01), except for the nearest part, i.e., the proximal, superficial, and lateral ones. Indeed, this lateral portion was significantly different in respect of the proximal and deep parts and of distal and superficial parts, but not if matched with the distal and deep parts. To the opposite side [Table 3]; from row E to row H, there were no differences among the distal parts ( P = 1.00).
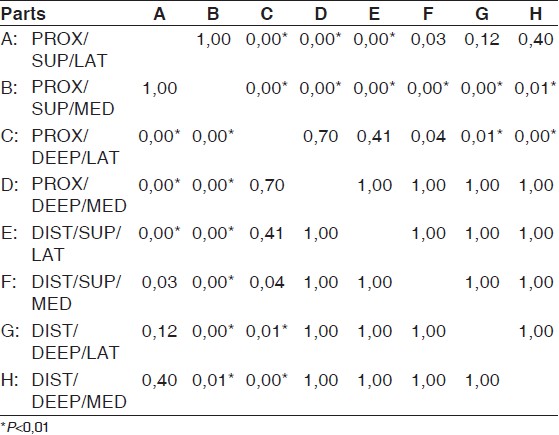
Table 3: Post hoc matches (Bonferroni method) for the eight coracoid parts (P<0.01)
The match between the normalized mean percentage of reabsorption of the 8 parts for the present study and those of the previous study showed a significant difference for the deep and lateral part of the distal coracoid bone graft (t value = 4.04; P < 0.01) and for deep and medial part of the distal coracoid bone graft (t value = 3.89; P < 0.01). In effect, in the present study, the mean reabsorption was 64.0% for the deep and lateral part of the distal coracoid and 67.3% for the deep and medial part of the distal coracoid bone graft, while, in the previous study, it was 37.5% and 36.2%, respectively [Table 4].
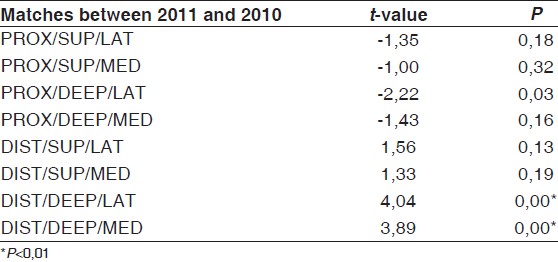
Table 4: Matches between the 8 coracoid parts of 2011 and 2010 (P<0.01)
Discussion
One of the causes of Latarjet procedure failure could be the progression of the transferred coracoid bone graft to osteolysis or fibrous union. [1],[2],[3],[5],[6],[10] Bone resorption study has been reported in the literature after 3 months and 8 months, respectively. [17],[18]
To our knowledge, there are no studies in literature that show the causes of coracoid bone graft osteolysis. Doursounian et al. performed a CT scan analysis in 11 of 34 patients treated with the Bristow procedure to study the position of the coracoid graft and to evaluate the presence of pseudarthrosis or osteolysis (pseudarthrosis was found in 4.3% of patients, coracoid bone graft osteolysis in 21.5% of patients). [19] Cassagnaud et al. performed a CT scan analysis in 80 out of 106 patients treated with the Latarjet – Patte procedure to assess the position of the bone block and the presence of osteoarthritis (osteoarthritis was present in 15% of patients, non-union in 7% of patients). [7] Di Giacomo et al. showed, using CT scan analysis, the position and the amount of the coracoid osteolysis in patient treated with the Latarjet procedure (on average about 60% of the coracoid process underwent osteolysis). [11]
None of this studies tried to understand the causes of osteolysis or non-union of the coracoid bone graft.
In this study, we tried to understand if modifying one of the biomechanical factors, the compression between the coracoid bone graft and the glenoid surface, could improve the bone healing and reduce the amount of coracoid bone graft osteolysis.
Because of the impossibility to change the patient’s biological factors, the authors tired to improve the compression between the coracoid bone graft and the glenoid surface using a mini-plate fixation technique.
This study revealed the coracoid graft region most involved in osteolysis is the proximal and superficial zone. On the contrary, all the distal region of the coracoid bone graft is the part least involved in osteolysis and have the best bone healing, with the only exception of the lateral part of the proximal and deep zone [Table 2].
We then compared our current results with the results from that of our previous study without using mini-plate fixation to determine if there is any statistical significant difference in terms of corcacoid bone graft osteolysis between the two surgical techniques for coracoid bone graft fixation.
These results find significant difference with the results of the previous study only for the deep part of the distal coracoid both lateral and medial, that seems to be more involved in osteolysis, even if these results did not correspond to any clinical findings.
The role of the bone block reported in the literature is controversial. [9],[20],[21] Thomas et al., [22] reported that there is no difference between the Bristow procedure and the conjoined tendon transfer alone in restoring anterior translation. Yamamoto et al., [23] concluded that the coracoid bone graft is the main factor for the stabilizing mechanism in patients with glenoid osseous defects.
In this study, despite the amount of osteolysis involving the coracoid bone graft (mean percentage 63.9%), there was no patient with recurrent shoulder dislocation and subtle instability. This reinforced the hypothesis that the coracoid bone graft is not the principal factor in the Latarjet procedure for antero-inferior shoulder stabilization.
According to the results of our study, we believe that the use of mini-plate fixation does not reduce the risk of coracoids bone graft osteolysis, even if we recommend the use of the mini-plate to improve the graft stability.
The limitations of this study were that it is difficult to understand whether the radiological findings noted indicate a real graft osteolysis or whether it is just a remodeling process of the coracoid bone graft due to the forces transmitted from the conjoined tendon and the humeral head onto the bony graft (Wolff’s law). The second limitation in this study is the low number of patients recruited due to the high cost of the CT scan examination.
Conclusion
To the best of our knowledge, this is the first study to determine if there is any statistical significant difference, in terms of corcacoid bone graft osteolysis, after the Latarjet procedure between the two surgical techniques for coracoid bone graft fixation.
Although the most relevant osteolysis was represented on the proximal part of the coracoid, osteolysis was also found on the distal part; this should be considered to be the most important for the bone-block effect.
The bone-block effect is an important factor in shoulder instability for patients with significant bony defects, but it may not be the main factor in patients without significant bony defects. Further studies are needed to understand the process of the coracoid graft osteolysis after the Latarjet procedure and ways to prevent and reduce this osteolysis process.
