Abstract
Purpose: The purpose of this study was to quantify the width of bone beyond the peak of the anterior glenoid rim and to determine if this anatomic region of the glenoid significantly affects measurement of the anteroposterior glenoid diameter.
Materials and Methods: 19 cadaveric scapulae were examined and the width of bone beyond the peak of the anterior glenoid rim was measured. The percent width of this region relative to the anteroposterior diameter of the glenoid was evaluated. Male and female specimens were compared. Measurements of the anteroposterior diameter of the glenoid, both including and excluding this region, were compared.
Results: The mean width of bone beyond the peak of the anterior glenoid rim was 3.2 ± 0.7 mm, corresponding to 10.5% of the anteroposterior glenoid diameter. This anatomic region is of similar relative size in males and females (11% vs 10% of the glenoid diameter). Measurement of the anteroposterior diameter of the glenoid is significantly different depending on whether this region is included or not ( P = 0.0064).
Conclusions: There exists a portion of the anterior glenoid that is beyond the peak of the anterior rim, and is not part of the concave articular surface. The width of this anatomic area comprises a significant percent of the anteroposterior glenoid diameter, and should be understood when quantifying and describing anterior glenoid bone loss in cases of glenohumeral instability.
Clinical Relevance: Understanding of anterior glenoid anatomy is important in the evaluation of glenohumeral instability. The portion of glenoid bone beyond the anterior rim peak is likely important for its soft tissue attachments, but its contribution to bony stability may be misunderstood.
Introduction
Stability of the glenohumeral joint relies on normal glenoid bony architecture and soft tissue static and dynamic stabilizing structures. Specific descriptions of the glenoid morphology have increased our understanding of pathologic conditions of the shoulder. [1],[2] In cases of recurrent anterior glenohumeral instability, much attention has been placed on quantifying the size of anterior bony glenoid defects, and multiple methods of measuring glenoid bone loss have been suggested.
[3],[4],[5],[6] Patients with significant bone defects are less likely to have successful outcomes with arthroscopic soft tissue procedures, and may require reconstruction with open soft tissue procedures or bone graft using a coracoid transfer (i.e., Latarjet procedure), iliac crest autograft, or allograft. [7],[8],[9],[10] Although accurately estimating the amount of bone loss has significant implications for both future instability and the success of different surgical procedures, there is no universally accepted method of measuring glenoid bone loss.
Glenoid bone loss associated with glenohumeral instability is usually identified at the anterior portion of the glenoid, at the 3 o’clock position in a right shoulder. [11] Less severe cases will involve only the periphery of the glenoid rim, while more drastic cases can involve significant percentages of the glenoid diameter.
Normal glenoid morphology has been described as pear-shaped with the inferior portion having a larger anterior to posterior dimension. In cases of severe bone loss, the glenoid has an “inverted-pear” appearance. [12],[13] The diameter of this portion of the glenoid has previously been reported to be between 27.8 and 28.6 mm in males and 23.6 and 26.7 mm in females.
[14] The articular surface of the glenoid is concave. At the anterior rim of the glenoid, the peak of the concavity is reached, after which the rim slopes medially towards the glenoid neck. The gross morphology of the glenoid has been described; however, to our knowledge there are no studies describing the width of bone beyond the peak of the anterior glenoid rim.
The purpose of this study was to quantify the width of bone beyond the peak of the anterior glenoid rim. [Figure 1] is a schematic diagram showing the region of the anterior glenoid being evaluated. Our hypothesis was that the measurement of the anteroposterior diameter of the glenoid would be significantly different depending on whether the region of bone beyond the peak of the anterior rim was included or excluded.
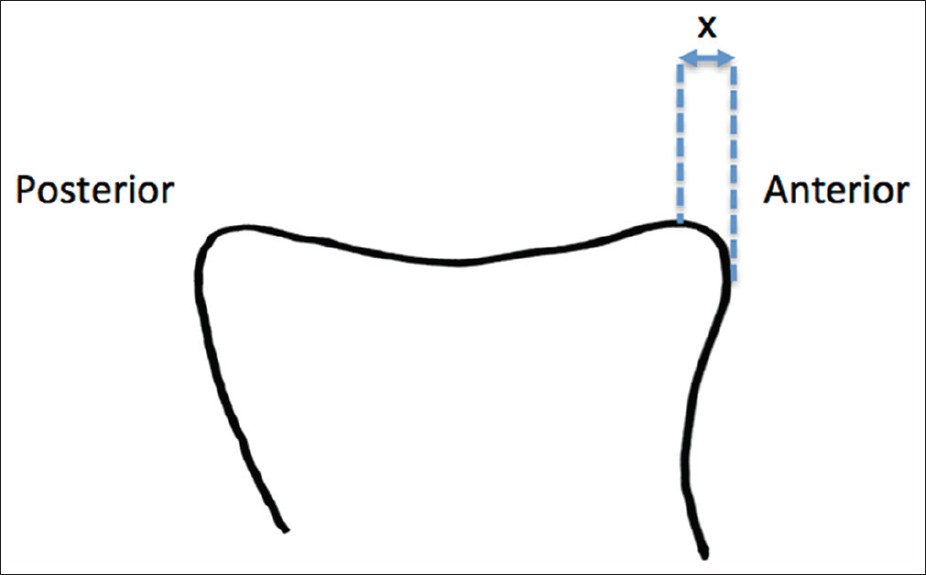 |
Figure 1: Axial schematic representation of the glenoid showing the presence of bone anterior to the peak of the anterior glenoid rim. “X” represents the width of bone anterior to the peak of the glenoid rim, which was measured in this study |
Materials and Methods
Nineteen right cadaver scapulae were obtained from our institution’s willed body program. Each scapula was dissected and the glenoid cleared of soft tissue structures, including the labrum. The age and gender of each specimen was noted. Using a digital caliper, the anteroposterior glenoid diameter was measured in millimeters (mm).
It was noted that the peripheral most portion of the anterior glenoid has a consistent change in contour. There is a “peak” beyond which the anterior glenoid rim slopes medially towards the glenoid neck. On each specimen, the anterior peak of the concave glenoid was noted, and the digital caliper was used to measure the glenoid bone anterior to this
. The width of bone anterior to the peak was expressed as a percentage of the anteroposterior diameter of the glenoid. Glenoid diameter including and excluding the measured width of bone beyond the peak of the anterior glenoid rim was compared using the student t-test for comparison of means.
The percent width of glenoid anterior to the rim peak was evaluated in male and female specimens and compared using the student t-test for comparison of means. Statistical significance was set at a P value of 0.05, with 95% confidence intervals.
Results
Nineteen specimens were evaluated. Ten specimens were male and nine specimens were female. The mean age of the specimens was 80.1 years. The mean age of the male specimens was 77.8 years, and the mean age of the female specimens was 82.6 years. No specimens had significant signs of osteoarthritis of the glenoid. The mean anteroposterior diameter of all glenoids was 29.9 ± 3.6 mm.
The mean anteroposterior diameter of male glenoids was 32.8 ± 2.1 mm and the mean anteroposterior diameter of female glenoids was 26.6 ± 1.2 mm (P < 0.05). The mean width of bone beyond the peak of the anterior glenoid rim was 3.2 ± 0.7 mm when evaluating all specimens. The mean width of bone beyond the peak of the anterior glenoid rim was 3.6 ± 0.6 mm in males and 2.7 ± 0.4 mm in females. Individual glenoid measurements are shown in [Table 1].
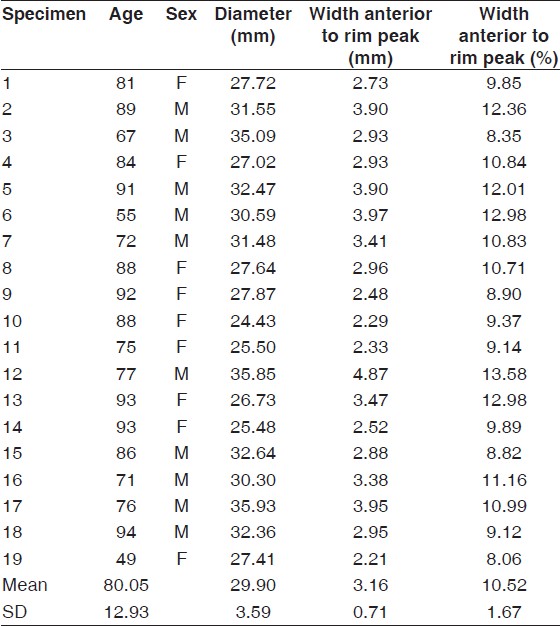 |
Table 1: Glenoid measurements |
The mean percent width of glenoid anterior to the peak of the anterior glenoid rim (width anterior to peak/anteroposterior glenoid diameter) was 10.5% ± 1.7%. The mean percent width of the glenoid anterior to the peak was 11.0 ± 1.8% in males and 10.0 ± 1.4% in females. There was no statistically significant difference between the relative size of this region in males and females.
The anteroposterior glenoid diameter was compared when including and excluding the width of bone anterior to the rim peak. The mean width of glenoid excluding bone anterior to the rim peak was 26.7 ± 3.1 mm. This was statistically different from the above reported mean anteroposterior glenoid diameter when the bone beyond the rim peak was included (P = 0.0064).
Segmented by gender, the mean anteroposterior diameter of the glenoid when bone anterior to the rim peak was excluded was 29.2 ± 2.0 mm in males and 24.0 ± 1.2 mm in females. This was statistically different from the above reported total anteroposterior glenoid diameter in each gender (P < 0.001 in each).
Discussion
The purpose of this study was to quantify the bone beyond the peak of the anterior glenoid rim, at the most peripheral portion of the anterior glenoid. We report statistically significant differences between the anteroposterior diameter of male and female glenoids, with males having significantly larger diameter glenoids. This is consistent with previously reported findings. [14]
All cadaveric specimens we examined had a similar change in the contour of the anterior glenoid from a concave articular surface that peaked and then sloped medially towards the glenoid neck. This portion of the glenoid has not been specifically described and quantified. The width of glenoid bone that lies beyond the peak of the anterior glenoid rim was found to comprise 10.5% of the overall glenoid diameter.
Although there is slight variation between males and females (11.0% in males versus 10.0% in females), this is not statistically significant. The 10.5% by which the anteroposterior diameter of the glenoid is increased by the width of bone beyond the peak of the anterior rim is statistically significant.
This anterior-most portion of the glenoid rim may not equally contribute to the congruity of the glenohumeral joint, and its loss may have less clinical impact than loss of bone more central on the glenoid. Bone loss more central on the glenoid face relative to this region diminishes the true diameter of articulating concave surface should theoretically bear more consequence in cases of anterior glenohumeral instability.
The work of Poppen and Walker discussed the importance of concavity-compression for normal glenohumeral motion. [15] Loss of glenoid concavity is an important factor contributing to glenohumeral instability. [16],[17] Although this study cannot comment on the biomechanical contributions of the bone beyond the peak of the anterior glenoid rim, in theory this bone does not contribute to glenoid concavity.
[Figure 2] shows three-dimensional reconstructions of an uninjured glenoid, viewed from different perspectives. Note the width of bone beyond the peak of the anterior glenoid rim, which is not part of the concave surface of the glenoid.
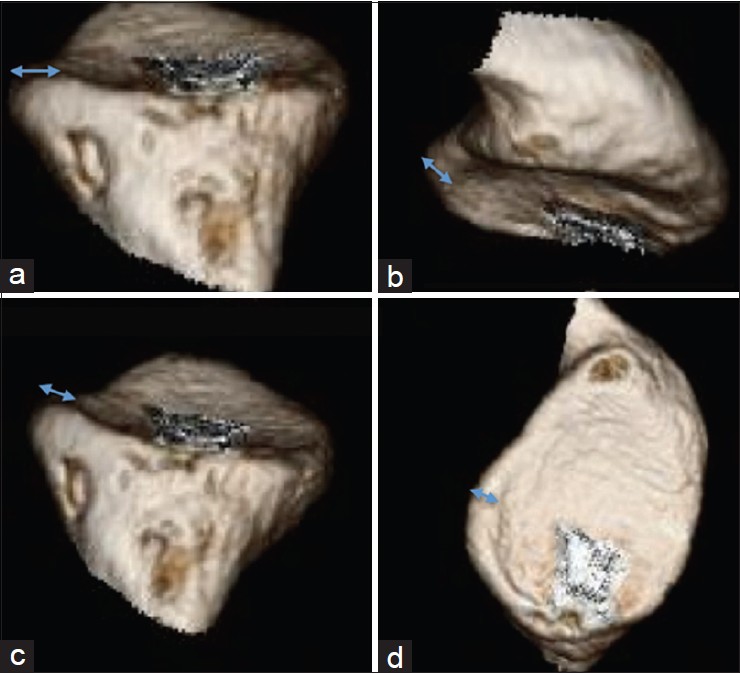 |
Figure 2: Various views from 3D CT reconstruction of an uninjured glenoid showing the presence of bone beyond the peak of the anterior glenoid rim. (a) View from inferior to superior; (b and c) Views from superior to inferior; (d) en-face view of glenoid |
The glenoid rim cannot be clinically evaluated at the exclusion of soft tissue structures that play a large role in glenohumeral stability. The anterior glenoid rim serves as the anchor point for the labrum, middle glenohumeral ligament, and inferior glenohumeral ligament. Although the width of bone anterior to the glenoid rim peak would not appear to contribute greatly as a bony stabilizer, its loss may compromise these soft tissue attachments.
The clinical importance of bone loss may not follow a linear algorithm, but instead perhaps increase in a more stepwise pattern once the anterior peak of the glenoid rim is lost. The role of this portion of the bony glenoid merits further evaluation to determine its contribution to stable, concentric motion of the glenohumeral joint.
Previously reported critical values of bone loss have been expressed one dimensionally and range between 21 and 36%. [13],[18] In a review article by Provencher et al., the critical limit is said to exist between 20 and 25% of the surface area of the best-fit circle of the inferior glenoid. [4] Many orthopedic surgeons currently use the best-fit circle technique described by Sugaya et al. to measure glenoid bone defects.
[19] The technique as described utilizes a ratio of the surface area of the glenoid defect and the surface area of a best-fit circle on the inferior glenoid to determine the percent size of the defect. When a best-fit circle is drawn on an en-face view of the glenoid on a three-dimensional reconstruction of a CT scan, the circle typically encompasses the entire inferior glenoid, including the width of bone that would lie beyond the peak of the anterior glenoid rim.
Given this, surgeons should understand this portion of the glenoid anatomy, and realize that bone loss comprising less than 10% of the diameter of the circle may not yet have breached the actual anterior peak of the glenoid rim.
Although Sugaya’s [19] described method utilizes a ratio of surface area (two-dimensional) to quantify bone loss, a one-dimensional measurement (the width of the bone defect divided by the diameter of the circle) is often used because it is simpler to calculate using commonly utilized imaging software than measuring area. [3] Unfortunately, the ratio of the surface area of the fragment to the surface area of the best-fit circle and the ratio of the width of the fragment to the diameter of the circle are not equivalent.
One-dimensional measurements overestimate the percent bone loss compared to two-dimensional measurements. [20] When using one-dimensional measurements, it would appear that the first 10% of bone loss would represent the portion of the glenoid anterior to the peak of the glenoid rim – thus bone beyond the concave articular surface of the glenoid.
The use of methods that quantify bone loss two dimensionally would decrease the relative percent size of the bone anterior to the peak of the rim. The relative area of the peripheral most segment of a circle represents a smaller percentage than the relative width of diameter of that same segment. Thus, the use of two-dimensional quantification techniques afford less relative size to the bone beyond the peak of the anterior glenoid rim, and may offer a more clinically appropriate method of describing the severity of anterior glenoid bony defects.
Using currently accepted methods of bone loss measurement, the region beyond the peak of the glenoid rim is included in measurement of the anteroposterior diameter of the glenoid. In corollary, if using two-dimensional measurement methods, this area is included in measurement of the surface area of the glenoid. However, unless measuring an uninjured glenoid, this region is usually not seen, given that the most anterior portion of the glenoid rim is the first to suffer injury in cases of anterior glenohumeral instability. The best-fit circle described above, which the physician uses to define the denominator for calculating glenoid bone loss, does include the region of bone beyond the peak of the glenoid rim.
Limitations of this study include the small sample size of the cadaveric specimens. The study is also unable to comprehensively evaluate the clinical relevance of the bone beyond the peak of the anterior glenoid rim. The evaluation of bony structures of the glenohumeral joint at the exclusion of soft tissue stabilizers cannot be considered complete.
Although we used cadaveric specimens to evaluate this portion of glenoid anatomy, imaging modalities such as computed tomography and magnetic resonance are typically used to measure the glenoid in the clinical setting. These modalities are considered precise and should reflect the true dimensions of the specimen; however, our study did not evaluate the specimens using imaging modalities and cannot comment on the applicability when measuring using imaging.
The average age of the specimens used in this study was above 80 years. The risk of osteoarthritis of the glenohumeral joint is increased in elderly populations, which could affect measurements of the glenoid; however, no significant signs of osteoarthritis were noted in any of the specimens.
Conclusion
The gross anatomy of scapula and glenoid has been described, but to our knowledge this is the first quantification of the width of bone beyond the peak of the anterior glenoid rim. Quantification of glenoid bone loss is important in preoperative planning for cases of anterior glenohumeral instability. The width of bone beyond the peak of the anterior glenoid rim is 10.5% of the anteroposterior diameter of the glenoid.
If included in measurements, this region of bone significantly increases the anteroposterior diameter of the glenoid. Although this region of the glenoid is an important anchor point for the anterior labrum, middle glenohumeral ligament and inferior glenohumeral ligament, it is not part of the concave, articular portion of the glenoid, and its role as a bony stabilizer may be misunderstood.
