1 Midwest Orthopaedics at Rush; Rush University Medical Center, Chicago, IL, USA
2 Orthopedic Center of Excellence, Columbus, OH, USA
Correspondence Address
Abstract
Operative treatment of displaced clavicle fractures has demonstrated lower rates of nonunion and symptomatic malunion, improved functional outcomes, and earlier return to activities versus nonoperative treatment. Surgical treatment may offer a reduction in the relative risk of nonunion and symptomatic malunion and an earlier return to work or sport. To present an easy and safe method of acquiring orthogonal views of the clavicle without any manipulation of the patient’s upper extremity. Academic medical center and private clinic in the Midwestern United States; retrospective patient cohort. We reviewed records of patients with acute clavicle fractures between January 2010 and August 2011. Thirty-four patients were treated with sling immobilization and 52 patients were treated surgically with superior plate and screw internal fixation. Prior to the introduction of orthogonal views, 19 patients were treated nonoperatively and 22 treated with internal fixation. Addition of orthogonal views increased the number of patients treated surgically: In the same period, 15 patients were treated nonoperatively and 30 with internal fixation. Following surgery, patients were evaluated in the outpatient office at 2 and 6 weeks and 3 and 6 months. Nonoperatively treated patients were evaluated at 1, 2, and 4 weeks and 3 and 6 months postinjury. Standard use of orthogonal views has led to greater utilization of surgical treatment of clavicle fractures at our institution and improved both the understanding and treatment of these injuries.
Keywords: Orthogonal x-ray, clavicle fracture, radiographic study
Introduction
Clavicle fractures are common, representing 2.6-12% of all adult fractures [1],[2],[3],[4] and 35-44% of all fractures to the shoulder girdle. [3],[5] Traditionally, these fractures were treated nonoperatively with expected good clinical and radiographic outcomes. It has been shown that patient-specific and fracture-specific factors such as increasing patient age, female gender, fracture displacement, comminution, and shortening are predictive of increased risk of symptomatic nonunion or malunion with nonoperative management [Table 1]. Early studies reported low rates of nonunion and high rates of satisfaction. [6],[7] However, more recent studies have demonstrated significantly greater nonunion (up to 15%) and symptomatic malunion rates with nonoperative management. [8],[9] Nonunions may be painful and functionally limiting. [2] These findings have prompted an increased utilization of surgical fixation of clavicle fractures. Further, operative treatment of displaced fractures has demonstrated significantly lower rates of nonunion [8],[9] and symptomatic malunion, [8],[10] improved functional outcomes, [8],[10] and earlier return to activities [10] versus that of nonoperative treatment.
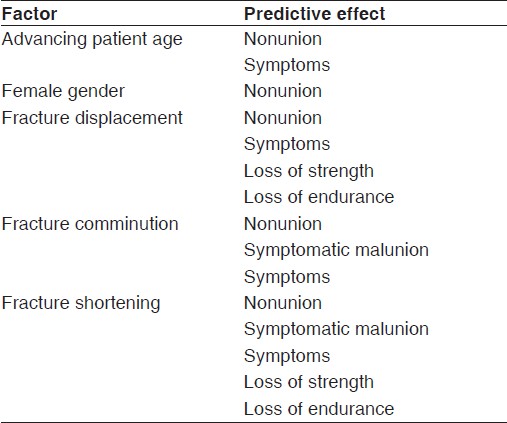
Table 1: Factors predictive of outcome following nonoperative management of clavicle fractures
The recommendation of surgical treatment of clavicle fractures is made on a case-by-case, individualized basis with a prerequisite discussion of the known potential risks and benefits of both operative and nonoperative management. Surgical treatment is an option that may be offered to patients within the premise of a reduction in the relative risk of nonunion and symptomatic malunion and an earlier return to work or sport. In most fractures of long bones, it is essential to gain orthogonal views of the whole bone to assess angulation, translation, and rotation. This sound management theory may apply to clavicle fractures, but traditionally nonorthogonal views have been used.
Currently, most published literature and orthopedic surgery textbooks do not recommend orthogonal views of clavicle fractures, and some even claim they are impossible to achieve due to thoracic structures obscuring the view. [11] Further, there is recognition that superimposed ends of a fracture on one view may appear united; however an orthogonal view may demonstrate residual displacement. [11] The authors of this manuscript recommend an easy and safe method of acquiring orthogonal views of the clavicle without any manipulation of the patient’s upper extremity. The authors hypothesize that the additional view serves three purposes that may improve upon the standard anteroposterior (AP) or posteroanterior (PA), minimally tilted (<30°) views: (1) Preoperative information relative to the amount of fracture displacement, shortening, and comminution. (2) Intraoperative information related to fracture reduction and plate placement. (3) Postoperative information relative to bridged cortices seen with fracture healing. Therefore, the clinical outcomes of patients managed with the additional radiographs described herein are being analyzed in a prospective validation study of the current pilot provisional study. Further, the additional radiographic information has improved both the understanding and treatment of these injuries. Herein is the description of proper technique of obtaining orthogonal views of the clavicle.
Technique
All clavicle and shoulder injuries that present to our institution are imaged with the patient upright, if possible. Supine radiographic examination alters the effect of gravity on fracture or joint displacement. All patients with known or suspected clavicle fractures or AC joint injuries receive an additional three views: (1) AP view of the clavicle [Figure 1] and [Figure 2], an orthogonal view taken at 60° above [Figure 2] and [Figure 3], and an orthogonal view 30° below the horizontal [Figure 2]. This series has been standardized at our institution and easily reproduced by all radiology technicians. These views are applicable with the patient standing with or without any immobilization device (sling, figure-of-eight dressing, or various other shoulder immobilizers). Thus, they are able to be utilized in the preoperative evaluation and postoperative assessment.
 Figure 1: Anteroposterior (AP) view of clavicle. X-ray beam directed perpendicular to coronal plane of body, while standing. X-ray cassette parallel to coronal plane of body
Figure 1: Anteroposterior (AP) view of clavicle. X-ray beam directed perpendicular to coronal plane of body, while standing. X-ray cassette parallel to coronal plane of body
![]() Figure 2: (a) AP view, with X-ray beam angled 30° superiorly (cephalic). (b) AP view, with X-ray beam angled 60° inferiorly (caudal)
Figure 2: (a) AP view, with X-ray beam angled 30° superiorly (cephalic). (b) AP view, with X-ray beam angled 60° inferiorly (caudal)
![]()
Figure 3: (a) Fluoroscopic image angled 30° superiorly (cephalic). (b) Fluoroscopic image angled 60° inferiorly (caudal)
In the operating room, these views are easily obtained with use of the mobile C-arm fluoroscopic unit [Figure 3]. The patient is placed in the semiseated position, with hips and knees flexed approximately 30°. Any radiographic image taken should be free of any metallic radiodensities that may obscure the view of the clavicle. The base of the C-arm is positioned on the contralateral side of the fracture. The image intensifier is placed beneath the patient, below the bed. The X-ray beam is produced above the patient, above the bed. A sterile C-arm cover is applied to this part of the machine, allowing it access to the surgical field and not risking contamination of the surgeon, the surgical assistant, or the field itself. In this position, the surgeon and surgical assistant may stand in the usual position at the side of the patient, anterolateral to the operative field. Orthogonal views may be taken without the surgeon or the assistant moving. The radiology technician only has to arc the beam 90° in the sagittal plane to obtain the two orthogonal views. These views may be taken prior to standard preparation and draping of the operative field to ensure adequate imaging may be obtained.
Patient series
The senior author’s (JCL; Shoulder and Elbow Fellowship-trained) practice primarily evaluates and treats shoulder and upper extremity injuries, both acute and chronic. From January 2010 to August 2011, all patients that presented to the senior author’s office or were evaluated and treated in hospital were analyzed. Inclusion criteria for reporting in this study were age greater than 18 years and an acute clavicle fracture (ICD-9 [International Classification of Diseases] code 810.0x) that was treated via CPT (Current Procedural Terminology) code 23500 (closed treatment of clavicle fracture, without manipulation) or 23515 (open treatment of clavicle fracture, includes internal fixation, when performed). Exclusion criteria were age less than 18 years or concurrent neurovascular injury. The introduction and standard use of this study’s proposed clavicle views have demonstrated better fracture anatomy characteristics. The ability to see anterior or posterior comminution or displacement that was previously less well visualized on typical clavicle series was greatly improved. Based on these criteria, 34 patients were treated with sling immobilization and 52 patients were treated surgically with superior plate and screw internal fixation. Prior to the introduction of orthogonal views, 19 patients were treated nonoperatively and 22 treated with internal fixation. Addition of orthogonal views increased the number of patients treated surgically: In the same time period, 15 patients were treated nonoperatively and 30 treated with internal fixation. Following surgery, patients were evaluated in the outpatient office at 2 and 6 weeks and 3 and 6 months. Nonoperatively treated patients were evaluated at 1, 2, and 4 weeks and 3 and 6 months postinjury.
Discussion
We have presented a technique that completely assesses the radiographic characteristics of clavicle fractures. A need existed to obtain all the pertinent information regarding fracture location, direction, displacement, shortening, comminution, and healing. An operative strategy cannot be confidently undertaken without having all the information, nor can the appraisal of fracture healing with or without operative intervention. In order to better evaluate fracture personality, we devised a standardized clavicle fracture series with orthogonal views that may be safely and easily acquired without any manipulation of the ipsilateral upper extremity. This series has been used successfully at our institution for one year. The introduction of these orthogonal views has changed our treatment pattern to address more clavicle fractures operatively. Only after an informed discussion with the patient about the risks, benefits, and expected outcomes of both nonoperatively and surgically treated fractures was operative intervention undertaken. It must be emphasized that this study is a pilot provisional study with introduction of a new radiograph. Based on the encouraging preliminary results, the authors are now prospectively analyzing patient outcomes with a validation study to be subsequently reported.
This view was initially used to better evaluate acute clavicle fractures in the decision-making discussion with the patient. Several patients had traditional AP views of the clavicle (separate by 30° of cephalic tilt) that demonstrated minimal superior or inferior displacement and looked relatively well aligned on both views [Figure 4]a and b. Thus, it was possible that an apparently minimally displaced fracture on standard AP views may be displaced significantly in the axial plane (anterior to posterior). This is a valuable component of an informed consent process if we are to truly describe displacement and comminution of a fracture [Figure 5]a and b. Patients need to have all the relevant pieces of information regarding radiographic characteristics of their injury in order to make a decision with their surgeon. Further, the surgeon has all the information to recommend with greater confidence the decision to proceed with surgery if indicated. In addition, recent studies have shown that up to 2/3 of initially minimally displaced fractures (less than 2 cm shortening) may progressively displace (to greater than 2 cm shortening) in the horizontal plane (not used in the study, but would have been optimally assessed with our orthogonal views) over a mean of 14.8 days postinjury with nonoperative treatment. [13] Of this latter group, many went on to surgical intervention. This further warrants serial radiographic examination, especially with orthogonal views.
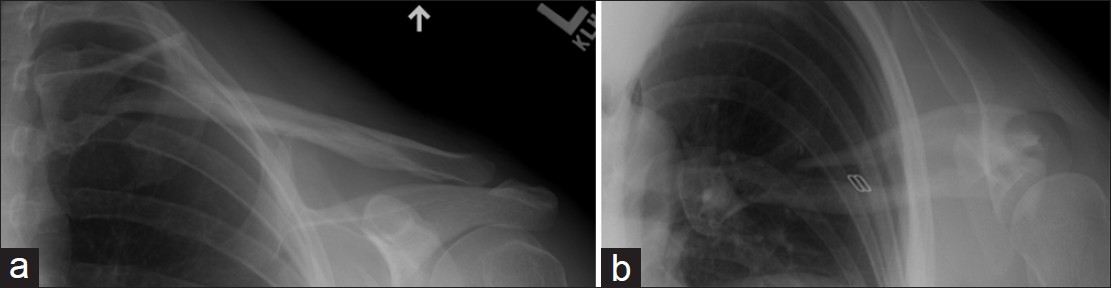
Figure 4: (a and b) Orthogonal views of medial clavicle fracture. Without the 60° caudally angled view, the long oblique fracture line would have been easily missed
Figure 5: (a and b) Orthogonal views of comminuted, segmental clavicle fracture. The AP view illustrates approximately 100% displacement with an irregular complex appearance of the medial aspect of the lateral fracture fragment, not clearly depicting this area.
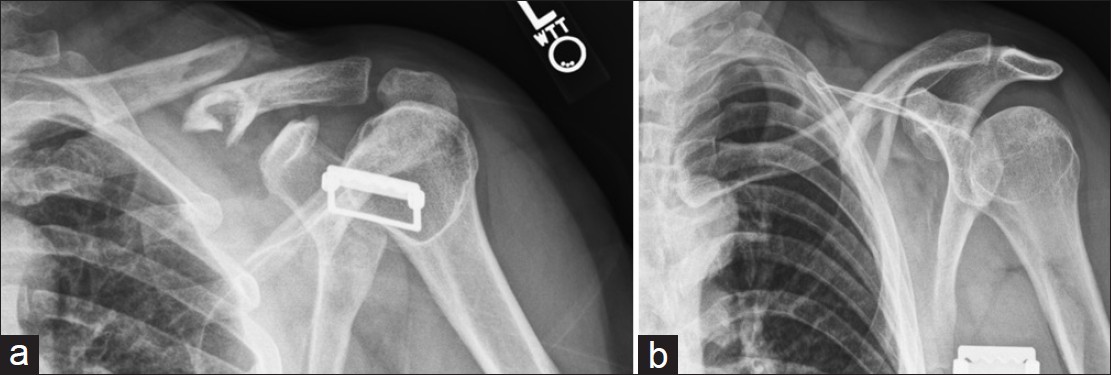
The 60° caudally angled view identifies a segmental fragment that is angled more in the sagittal plane, plainly seen as the round tubular structure of the midshaft of the clavicle on the traditional clavicle AP view. This segmental fragment could have been easily missed without the former view
If surgery is chosen, these orthogonal views may be easily integrated into the operative theatre without any significant increase in radiation exposure and any increase in risk of sterile field contamination. Despite the open nature of surgical treatment and direct visualization of superior plate placement, the addition of one C-arm fluoroscopic image adds minimal additional exposure to the site and the operative theater, while adding significant confidence in plate location and screw placement. If ESIN (elastic stable intramedullary nailing) is chosen surgically rather than a plate/screw construct, the use of orthogonal views may reduce the significant learning curve that is associated with increased radiation exposure. [14] It is especially useful for mid-distal 1/3 fractures in which plate selection and the potential ability to even use a plate was in question. Given the known sigmoid anatomy of the clavicle, which changes from circular at mid-shaft to flatter in the axial plane at the distal end, there is ample room to place several screws distally through an accommodating plate despite an AP view that demonstrates little room distally. With several newer anatomic plate designs on the market, distal locking screw options allow for the placement of anywhere from three to eight screws in the distal fragment of a distal 1/3 fracture. Without orthogonal views, extensive acromioclavicular (AC) joint ligament stripping would be required to visualize this intraoperatively and then make a decision whether plate placement was possible. Our radiographs gave us the confidence to take down the AC ligaments to place a plate/screw construct, and then repair the ligaments after.
Following surgical or nonsurgical treatment, the same radiographic characteristics of the fracture can be assessed to estimate fracture healing. This is especially useful if the patient has persistent pain following nonoperative management, indicative of potential symptomatic malunion or nonunion. At our institution, we generally obtain the orthogonal clavicle series at the first postoperative visit. At this point, the patient is in a sling. Our radiographic views do not require any arm manipulation, thus not stressing the fixation construct at all. Patients seem to appreciate seeing the two orthogonal views and better understand their injury and how it was treated. As surgeons, we have come to understand plate placement better in the axial plane when we visualize these films.
Radiographic views, such as the abduction lordotic view, apical oblique view, and Quesada views have been described to assist in clavicle fracture evaluation. The abduction lordotic view is obtained with arm abduction to 135° and the X-ray beam angled 25° cephalad. [15] This view is impractical in the acute setting with injury and intraoperatively. The apical oblique view is obtained by angling the patient’s injured side toward the X-ray beam 45° and the X-ray beam angled cephalad 20°. [16] This view is best utilized for nondisplaced neonatal clavicle trauma [16] and has been shown to be less effective than even a standard AP view. [17] Further, the apical oblique view is more appropriate as a tool to assess glenohumeral joint anterior and posterior instability, glenoid fractures, and Hill-Sachs defects. [18] Quesada views were originally described in 1926 as 45° caudad and 45° cephalad views (true orthogonal views). [19] Although would provide true orthogonal projections, these views have not been integrated into clinical practice in nearly 100 years. Many references conclude that a single AP with or without the addition of a 20° cephalic tilt film provides adequate information without interference by thoracic structures. [20]
This manuscript simply introduces the technique of acquisition of orthogonal views of the clavicle in the pre-, intra-, and postoperative settings. While these views lack validation in the ability to detect a significant difference in the need for surgical intervention and subsequent clinical outcomes, we have demonstrated that our treatment strategy has favored operative intervention with introduction of a complete clavicle radiograph series, based on numbers of patients treated nonoperatively and surgically. Although surgical treatment is increasingly used, the clinical outcomes of these patients have yet to be elucidated. This is a current topic of investigation at our institution. This study is moreover limited in that a gold standard of assessment of displacement, shortening, and comminution of clavicle fractures does not yet exist to make a valid comparison. In addition, intra- and interobserver performance reliability has yet to be demonstrated. While it is recognized that many surgical treatment options exist to treat clavicle fractures, including different plate and screw constructs (such as the ones used in this study), other options are widely used internationally, including ESIN. Although not evaluated specifically for the purposes of this study, we speculate that the addition of intraoperative orthogonal views would provide substantial benefit in intramedullary nail placement, potentially reducing operative time, avoiding aberrant nail placement, and obviating an incision over the fracture for reduction. Further, these views assist in selection of implant (plate and screws versus ESIN) as ESIN may not be ideal for fractures with significant comminution. These are all topics of current research at our institution.
Conclusions
An easy and safe method of acquiring orthogonal views of the clavicle without any manipulation of the patient’s upper extremity has been presented. The additional view serves three purposes that improve upon the standard AP or PA, minimally tilted (<30°) views: (1) Preoperative information relative to the amount of fracture displacement, shortening, and comminution. (2) Intraoperative information related to fracture reduction and plate placement. (3) Postoperative information relative to bridged cortices seen with fracture healing. The standard use of these views has led to greater utilization of surgical treatment of clavicle fractures at our institution based on fully informed patient-surgeon discussions. The authors have used this radiograph without any difficulty by the radiology technicians in the clinic or the operating room. Further, it has improved both the understanding and treatment of these injuries. Encouraging preliminary results of the introduction of this newly described radiographic series in this pilot study has thus instigated a prospective validation outcomes study at our institution to be subsequently reported.
Acknowledgments
The authors would like to acknowledge and thank Bill Thorpe, Lisa Haubert, M.D., and Heather Hill for their assistance in imaging during the preparation of this manuscript.
